
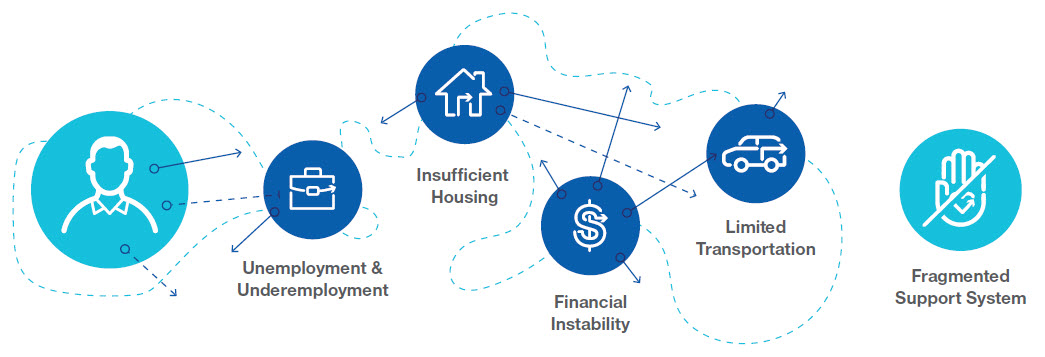
Many Medicaid members face significant challenges. In addition to the challenges of managing multiple behavioral and physical health conditions, many face social and economic factors--social drivers of health-- that impact their health and well-being. These include food insecurity, unsafe and unstable housing, lack of transportation, unemployment, financial instability and more. All of these factors can come between Medicaid members and their ability to receive the care they need – leading to increased ER utilization, poor outcomes and higher spending.
4 out of 5 physicians think patients’ unmet social needs lead to worse health outcomes
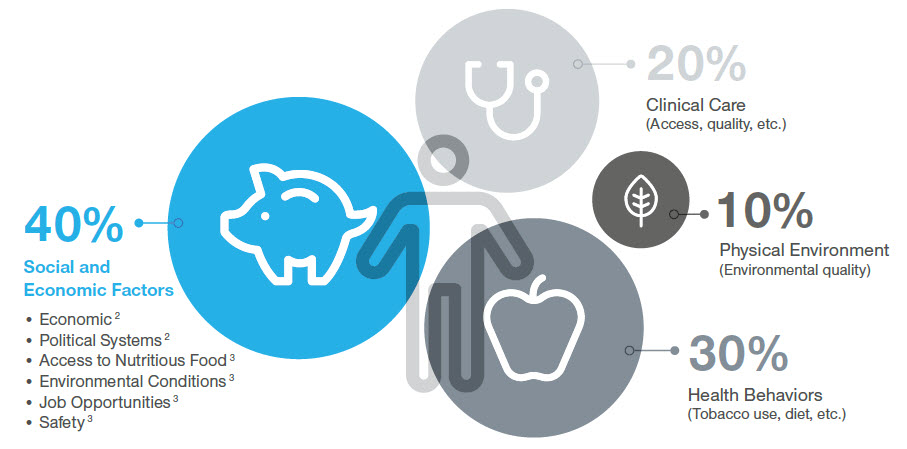
Studies show that taking a holistic view of members’ circumstances is important, given that social and economic needs have a significant effect on health outcomes. In fact, 4 out of 5 physicians think patients’ unmet social needs lead to worse health outcomes and are as important to address as medical conditions.
Addressing SDOH through services such as supportive housing and employment support is therefore of critical interest to states, health care providers and managed care organizations (MCOs). UnitedHealthcare Community & State has developed core service lines and capabilities designed to address social determinants holistically. Our goal is to improve access to, and delivery of, community resources that are the gateway to overall well-being and that ultimately impact health outcomes.
Key considerations when integrating services to address SDOH:
Data collection and sharing: Accurate data on the number of Medicaid beneficiaries with social service needs and specific vulnerabilities is needed to calculate changes in health outcomes, cost, and return on investment. It is equally important to be able to share data easily.
Disparate funding sources: Bringing together multiple funding sources requires trust between organizations and clear mechanisms to hold programs accountable and track funding, if necessary.
Varying philosophies: Bridging different agencies and organizations requires trust between “owners” of each service and the ability to balance different philosophies of care. Without stakeholder buy-in, coordinated delivery is not feasible.
Working with non-traditional providers: Creating strong partnerships with human service providers and community- based organizations (CBOs) is critical to success. Ideally, MCOs will be able to track referrals to CBOs and services delivered to accurately understand the care being delivered.
Examples of state SDOH action:
