Individuals with intellectual and developmental disabilities, physical disabilities, behavioral health issues, cognitive impairments (e.g., Alzheimer’s or dementia), or serious mental illness often require long-term services and supports (LTSS).
LTSS includes an array of health and social services that help support these individuals with activities of daily living (ADLs), such as bathing, eating, and toileting, as well as instrumental activities of daily living (IADLs), such as medication management, budgeting, and transportation.
Individuals receive these services in a variety of settings, ranging from institutional facilities such as nursing homes or intermediate care facilities to congregate settings including assisted living centers and group homes to privately-owned homes or apartments.1
Over the last several years there has been an increased emphasis on home and community-based services (HCBS). States and the federal government have begun to work towards increasing access to HCBS to better manage care for consumers using LTSS and improve patient experience, quality of life, and health outcomes. HCBS has also been shown to be less costly than institutional care. It is generally accepted that three individuals can receive HCBS in the community for the cost of serving one person in an institutional facility.² This makes HCBS an appealing option for states as health care costs continue to rise.
As the primary payer and source of health care coverage for individuals with complex health conditions, Medicaid has a vested interest in designing programs that improve their quality of care while addressing the high cost associated with serving these individuals. Working in partnership with the Centers for Medicare and Medicaid Services (CMS), states are working towards designing programs that deliver high-quality systems of care for individuals with complex care needs.
Overview of the project and methodology
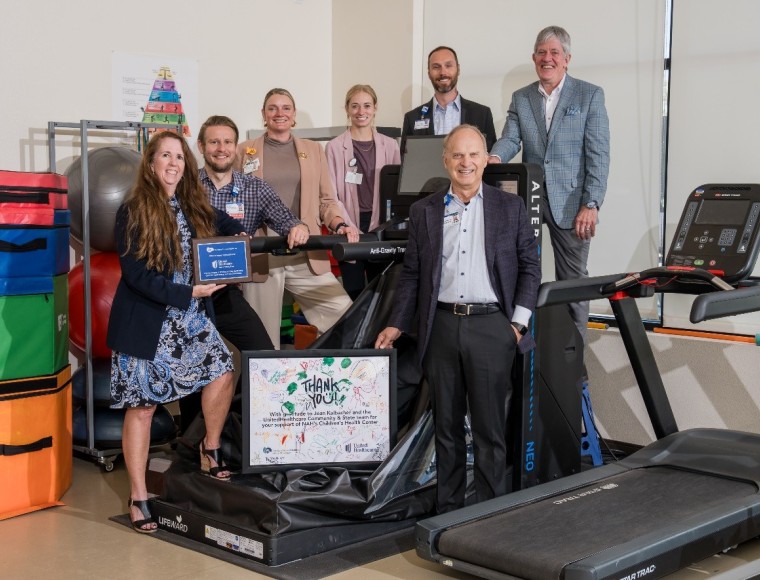
UnitedHealthcare Community and State (UnitedHealthcare), in partnership with its independent National Advisory Board, has undertaken a multi-year project to explore data and research to develop recommendations for benefit designs that better support people with disabilities of all ages and their caregivers. The goal is to achieve improved health and wellness while affording them greater flexibility and control over their lives.
The Board is composed of leading experts in aging and disability policy and practice, a UnitedHealthcare health plan member and a family caregiver of a child with special health care needs. The Board provided UnitedHealthcare with guidance and input to promote a better understanding of the needs of individuals with disabilities of all ages and their family caregivers, and of the programs and services that can best support them.
The project focused on creating benefit and program design recommendations that support the following four population groups:
- Individuals with Alzheimer’s or related dementias
- Individuals with physical disabilities
- Individuals with intellectual and developmental disabilities (I/DD)
- Individuals with behavioral and mental health conditions (including Serious Mental Illness and Substance Use Disorder (SUD))
The following conclusions and recommendations reflect the Board’s input and guidance. These recommendations are based on analysis of Medicaid waivers, including Section §1915(b), §1915(c), and §1115 demonstration waivers for all 50 states, Puerto Rico, and the District of Columbia, as well as state plans, where readily available. Additional information from published literature and other reports, along with the team’s waiver knowledge, were also used to support this initiative.
The Board’s recommendations aim to:
- Be person-centered;
- Support a holistic view of sustainable long-term health and well-being rooted in communities; and
- Serve individuals in a culturally-competent manner
UnitedHealthcare is committed to leveraging the research and recommendations associated with this project to support individuals with chronic and/or disabling health conditions and their caregivers.
Medicaid state plans and waivers
While federal regulations set the requirements for state-operated Medicaid programs and mandates coverage of some populations and certain benefits, many coverage and benefit decisions are up to the individual states. For example, states decide who is eligible beyond mandated populations, which optional services will be covered, and what the payments for services will be. Figure 1 compares the mandatory benefits that states are required to cover per federal regulations and the optional benefits that are at states’ discretion. Each state is required to submit a comprehensive document to CMS outlining the scope of its Medicaid program in its State Plan.
Figure 1: State Plan Benefits: Mandatory and Optional 3
State plan services and eligibility options are entitlements, and the state plan prohibits states from establishing annual benefit maximums for an individual, setting enrollment limits, or maintaining waiting lists.
However, states that want additional flexibility to design different benefit packages for specific populations, to restrict individuals to certain providers, or to extend coverage to groups beyond what is defined in Medicaid law can apply for a waiver of the federal Medicaid statute.
Some of the most common waivers that states leverage include the following:
- §1115 demonstration waivers
- §1915(b) waivers
- §1915(c) waivers
Figure 2 provides details on the differences between the state plan and the most commonly used Medicaid waivers.
Figure 2: Comparison of State Plan and Various Medicaid Waivers 4
Waivers can help states accomplish a number of different objectives, including:
- Providing benefits that are targeted to specific groups of individuals based upon diagnosis, disability, and/or geographic regions;
- Expanding eligibility to groups not traditionally covered by Medicaid;
- Experimenting with new service delivery methods or benefit design; or
- Enrolling individuals into managed care plans
States leverage waiver flexibility to customize their Medicaid programs to meet their unique needs. This flexibility allows states to make decisions about their specific program design, inclusive of eligibility, delivery system, premiums and cost sharing, and optional benefits. For LTSS, many states have designed waivers that allow them to provide services to individuals at home or in the community instead of in institutional settings, allowing individuals to remain as independent as possible.
All 50 states use some type of waiver authority to provide HCBS benefits to individuals, and in some instances, their caregivers. However, the number, type, and scope of Medicaid waivers vary considerably across states. Most states use §1915(c) waivers to meet the needs of people in need of LTSS in their home or community instead of an institutional setting or long-term care facility. Some states also leverage §1915(c) waivers to provide respite care, training, and family counseling. In waiver programs, many states permit individuals to hire family members as caregivers directly.
The majority of states currently elect to provide HCBS benefits through §1915(c) waivers. An alternative to using §1915(c) waivers to provide HCBS benefits is through §1115 demonstrations. Rhode Island and Arizona are among the states that utilize this flexibility.
Designing benefits to support individuals with complex needs
HCBS benefits should provide maximum flexibility to enable persons with complex health needs to live with dignity and independence in the community by expanding, strengthening, and integrating systems of community-based long-term supports that are person-centered.
The majority of the LTSS that aide individuals with functional limitations should be available to all waiver recipients, regardless of diagnosis. States can also choose to target benefits to specific populations based on functional diagnosis and in accordance with their person-centered plan. This would allow states to limit access to those who actually need these supports through state-defined medical necessity criteria. For example, individuals with physical disabilities may not need benefits such as assertive community treatment (ACT) or dialectic behavioral services; whereas, individuals with serious mental illness are likely to benefit from these services.
Benefit designs should reflect that individuals are unique and come from a variety of backgrounds. Each state has a different demographic set of ethnic, racial, religious, geographic, or social minority groups—many of whom experience unequal access to and outcomes from HCBS systems. The decision-making authorities in each state are trusted to develop and exercise their cultural competency when creating waiver systems. Effective cultural competency goes beyond merely identifying the needs and values of individuals with diverse cultural backgrounds; plan designers must treat these differences respectfully and actively work to address these differences in the fundamental structures of the waiver systems they create.
UnitedHealthcare and its Board recommend that states make available the benefits and services shown in Figure 3 to all individuals in need of LTSS. States should provide these benefits to individuals based on their needs and desires and in alignment with their person-centered care plan (and not solely on diagnosis).
Figure 3: Person-Centered Benefit Design Recommendations for All Populations Needing LTSS
In addition to the comprehensive benefits to be offered to individuals who are in need of LTSS, UnitedHealthcare and the Board recommend that states offer additional benefits to individuals with certain functional diagnoses and in accordance with their care plan, which are detailed in Figure 4.
Figure 4: Additional Benefit Design Recommendations for Individuals with Intellectual Disabilities and Developmental Disabilities, Behavioral and Mental Health Conditions, and Alzheimer’s or Related Dementias
The Appendix provided at the end of this document includes general definitions of all of the benefits listed in Figures 3 and 4.
Leveraging Medicaid waivers to support state priorities
Administrative requirements for Medicaid waivers
While Medicaid waivers provide states with additional flexibility to design programs that differ from what is required by federal rules, the administrative requirements that accompany applying for and implementing these waivers are extensive. States seeking to leverage waiver flexibility must develop waiver requests and submit them to CMS. CMS requires significant stakeholder engagement on all waivers. For §1115 demonstration waivers, states must meet certain transparency requirements before submission, which usually involves holding a public comment period. States must also obtain public input during the development of §1915(b) or §1915(c) waivers and make the waiver draft publicly available prior to submission.
After the prerequisites for the waiver request are met, the state must then submit the request to CMS. The approval process varies by the type of waiver. While CMS has at least 90 days to approve §1915(b) and §1915(c) waivers, CMS usually takes much longer to review and approve §1115 demonstration waivers. As part of the §1115 demonstration waiver approval process, CMS and states often engage in prolonged negotiations, during which time the waiver request may undergo several changes. After a waiver is approved, states must evaluate their program and submit frequent (quarterly and annual) reports to CMS.
States that operate multiple waivers must undertake additional administrative responsibilities. As detailed above, each specific waiver requires its own application, must be renewed individually, and has separate and distinct reporting requirements, as mandated by CMS. States must also oversee multiple contracts and contractors, maintain separate systems and processes, manage multiple waiting lists and program budgets, and administer multiple quality programs, among other administrative tasks. Additionally, in many states, each waiver is managed by a different statewide administrative entity, which further complicates program administration.
Achieving administrative effectiveness
Despite the administrative complications associated with operating multiple HCBS waiver programs, most states still use multiple waivers to provide HCBS to individuals in need of LTSS.
Federal authority, however, provides states with the flexibility to serve individuals of different target groups under one waiver.⁵ On January 16, 2014, CMS published a final rule (42 CFR 441.301 (b)(6)) that permits states to combine target groups within one waiver, removing a barrier for states that wish to design a waiver that meets the needs of more than one target population. The provision of the rule related to target groups provides an option to states to design services across populations, which may lead to improved integration and administrative efficiencies in state Medicaid agencies.
To operate under this rule, a waiver must be limited to one or more of the following target groups or any subgroup thereof that the state may define:
- Aged or disabled, or both
- Individuals with Intellectual or Developmental Disabilities, or both
- Mentally ill
Through this guidance, CMS was attempting to create some standardization on key program elements related to policy objectives that are of importance to stakeholders, providers, and policymakers. The guidance was also intended to provide states with the flexibility needed to evolve their programs. Prior to this regulation, states were required to develop separate §1915(b) and §1915(c) waivers to serve more than one of the specified target groups; this resulted in states simultaneously operating numerous waivers, for example ranging anywhere from one to 11 §1915(c) waivers in a single state.
Despite this flexibility, many states still administer several waivers to provide services to a variety of populations. In addition to the administrative burden that administering multiple waivers creates, it also causes confusion for individuals in need of services, and often results in misalignment of services to individual needs.
Recommendations
Streamline and consolidate existing waivers
States should look for opportunities to streamline and consolidate their existing waivers to create program efficiency by decreasing the administrative complexity inherent when operating multiple waivers.
The current Medicaid HCBS system creates confusion for individuals in need of services. Individuals seeking services have to navigate the program’s complexities, which include different benefits and eligibility requirements, in order to determine which program best meets their needs. Creating a system that is easy to navigate facilitates the ability for individuals to get the services and information they need and improves consumer experience.
For example, one benefit package may include personal care for people with physical limitations, while another benefit package may provide specialty behavioral health services. If different services are offered through distinct programs, people with multiple needs will have to choose which services to pursue and which to forgo.⁶ There are many benefits to streamlining Medicaid HCBS programs into a single waiver, including:
- Allows states to serve individuals of different target groups who live together (e.g. an individual with an intellectual disability and his/her aging parent) seamlessly
- Reduces administrative costs and frees up funds for the provision of services with no bottom line impact to the overall state budget
- Recognizes that individuals’ needs may make them eligible under multiple eligibility groups and offers an array of services to meet a wide arrange of needs, regardless of diagnostic category
- Encourages person-centered approaches to care by enabling alignment of services to specific needs rather than aligning to specific waiver design
- Encourages administrative efficiencies for states that offer the same benefits to multiple target groups using multiple waivers
- Decreases administrative complexity for states by moving away from a piecemeal approach, as they will not have to combine multiple authorities, administer different sets of eligibility rules, and oversee distinct quality measures
Ensure program design simultaneously improves care and contains costs
While there are several advantages for states opting to consolidate their waivers, states must also ensure that their program design recommendations simultaneously improve care and contain costs. Federal regulation requires that states must demonstrate cost neutrality in their waivers, while emphasizing preventative care and keeping people healthy. Cost neutrality requires that spending on waiver services cannot be greater than they would be in the absence of the waiver. States considering consolidating multiple HCBS waivers must carefully weigh cost neutrality requirements and long-term program savings against the administrative efficiencies achieved through waiver consolidation. When designing programs, states should make investments in quality care upfront in order to ensure the cost-effective use of resources.
Strengthen self-care supports for caregivers
Caregivers face a number of challenges. It can often be difficult for them to find time for themselves, potentially leading to fatigue, distress, or health issues of their own. Existing Medicaid authorities can be used to strengthen caregiver supports, especially §1915(c) waivers. Waivers allow states to provide support to caregivers including respite care, training and educational opportunities, and counseling. Ensuring caregivers are supported will positively affect the individuals they are caring for. Therefore, assuring that caregivers are aware of these resources is critical.
Guarantee programs are in alignment with federal guidelines
As states consider consolidating or streamlining their waivers to customize their programs and provide a defined set of HCBS to targeted populations, states must ensure the following:
- Each individual within the waiver, regardless of target group, must have equal access to the services necessary to meet their unique needs as indicated in the person-centered plan; and
- States may not limit services based on an individual’s target group; for instance, states cannot mandate that the Personal Emergency Response Systems (PERS) benefit is only for older adults or that individuals with I/DD can only access habilitation services.
Conclusion
As states continue to navigate complex political and budgetary environments, they along with CMS continue to look for ways to improve the availability and delivery of LTSS. It is imperative that the federal government, states, stakeholders, beneficiaries, and insurers work together to design programs and provide benefits that are most appropriate for individuals with complex health needs.
UnitedHealthcare and its National Advisory Board are dedicated to ensuring that individuals of all ages with intellectual and developmental disabilities, physical disabilities, behavioral health diagnoses, cognitive impairments, or serious mental illness have access to the services they need to live healthier lives in the community as well as greater flexibility and control over their own lives.
Sources
- C. Dobson, S. Gibbs, A. Mosey, and L. Smith. Demonstrating the Value of Medicaid MLTSS Programs. National Association of States United for Aging and Disabilities (NASUAD) MLTSS Institute. May 2017
- “Providing More Long Term Support and Services at Home: Why It’s Critical for Health Reform.” Fact Sheet. AARP Public Policy Institute. 2009
- “Mandatory & Optional Medicaid Benefits,” Medicaid.gov, Centers for Medicare & Medicaid Services
- Adapted from https://www.macpac.gov/topics/waivers/ and Information from Medicaid.gov
- A provision of the 2014 1915(c) HCBS Final Regulation permits states to serve multiple target groups under one 1915(c) waiver.
- Streamlining Medicaid Home and Community-Based Services: Key Policy Questions
- Peebles, Victoria and Alex Bohl. “The HCBS Taxonomy: A New Language for Classifying Home and Community Based Services.” Centers for Medicare and Medicaid Services Medicaid Policy Brief. Brief 19. August 2013.